Dec 9, 2021 Society
Everything we do as a society relies on a shared conceptualisation of what ‘society’ is.
It is easy to assume ‘we’re all in this together’, but without true commonalities we are strangers forced together by coincidence, colonisation and coercion.
To achieve anything together, we must feel like we are truly together. There needs to be trust. Trust isn’t inherent, it is something that is hard to earn, easy to lose, and requires maintenance.
New Zealand government agencies have, since their inception, maintained trust amongst Māori like a negligent landlord maintaining a dodgy rental property with water pouring from the walls and black mould coating the throats of its unlucky inhabitants — intentionally poorly, while draining out every dollar they can.
If you are a public health leader in this country, legal action and court judgments against you are a regular occurence in your life. Whether from Māori health providers, people with disabilities and their families, or even the United Nations, our health system is regularly on the wrong side of both history and legal judgments.
As you read this, New Zealand’s health system is breaching the United Nations Convention on the Rights of Persons with Disabilities and the Convention against Torture and other Cruel, Inhuman or Degrading Treatment or Punishment. We were among the first nations to sign up to these human rights protections in front of the world while bragging about our moral superiority, and we have been in breach ever since.
Albert Einstein once said (possibly apocryphally), “Insanity is doing the same thing over and over and expecting different results.” An accurate update of the phrase for our public health system would be: “Insanity is doing the same thing to the same whānau over and over and telling them to expect different results.”
Māori may suffer from mental health issues at a staggeringly high rate, but believing everything the public health system claims would be mass delusion. It would be a mental health pandemic. So why would I trust the system now?
To fully answer this, we first need to understand our national history of failures. Only then will we be able to move beyond ‘us’ and ‘them’ narratives towards something more tailored which reflects, acknowledges and learns from past errors.
We take their ‘cures’, while they suppress our medicine
If there can be an identifiable ‘original sin’ which began the distrust we find ourselves dealing with today, it would be the Tohunga Suppression Act 1907.
The Tohunga Suppression Act was created to discredit and criminalise traditional Māori health practices. The intended effect of this was to ensure the government’s health system faced no competition or alternatives. The Act was not very effective in its prosecutions — only nine convictions were ever obtained — but it was highly successful at sowing the seeds of distrust in traditional Māori values.
In effect it ensured that Māori gave up on our own conceptualisations of ourselves — Māori well-being traditionally required more than just a single healthy body with no connection to the health of the whānau and environment.
While twisting and relabelling the care for loved ones and the waterways that fed them as the product of a ‘primitive’ mindset, the Western model of healthcare has also since its forced introduction to this country sought to remove whakapapa from the conceptualisation of good health. Māori have been stripped of their identity and forced to become mere numbers in a “team of millions”. Silent team members, ideally.
This effort to put down Māori heath practices worked as intended, but there was one inconvenient fact — health outcomes for Māori didn’t improve, and have continued to lag behind progress made by non-Māori since 1907.
Ignoring our shared history
Even after tohunga were outlawed, health services to replace the now-banned traditional Māori knowledge were few and far between, with none designed with Māori or with equity of outcomes in mind.
The 1918 influenza epidemic devastated Māori communities (many of which have struggled again during the current pandemic), due to their living mostly on regional rohe and not in urban settings where healthcare services were then (and remain) focused. With health services built nearby and designed to reflect their personal preferences, Pākehā were seven times less likely to die than those in Māori communities.
Urupā in regional Māori communities are littered with cautionary tales against taking an epidemic lightly, but the outcomes and the solutions designed over 100 years ago and share unfortunate similarities with those of today. These being a focus on a ‘with-us-or-against-us’ rhetoric, and a focus on urban settings. It should come as no surprise that the District Health Boards with the highest vaccination rates are located in Auckland and Wellington.
If this shared history had been considered before the public campaign against Covid, the messaging and emphasis may have been different. Sadly the history of public health in this country is littered with ignored warnings, primarily from Māori, but also from global health leaders and the United Nations.
Isolation and torture: a disproportionally Māori issue
Torture is a big and evocative word with negative connotations. International human rights observers avoid using it flippantly, as there can be huge differences in terms of long-lasting damage from one breach to the next. Like the old anti-piracy ads which noted jokingly “You wouldn’t download a car”, there can be false equivalence issues around human rights breaches.
In 2016 the United Nation General Assembly passed a non-binding resolution that declared “internet access a human right”; failing to ensure everyone has internet access is a ‘technical’ rule break from any nation who agreed to it. However there are no repercussions for failing to achieve the goal — it is essentially aspirational.
Other New Zealand breaches are a bit more serious — closer to what most people would conceptualise as torture based upon pop culture depictions. If you’re imagining Hannibal Lecter being rolled into a courtroom in a full straightjacket and face mask, you are quite close but overly kind.
Our health system’s frequent usage of the controversial practice of ‘seclusion’ — essentially isolating a patient in a locked secure room by themselves, potentially while restrained to a bed, for a matter of hours or days — is staggering. Seclusion isn’t kept for use only against serial-murdering cannibal super-villains, it is used mostly against non-criminal mental health patients. Some have intellectual disabilities. All are seeking help.
Wellington’s Haumietiketike, an intellectual disability forensic unit, was found this year to have kept an intellectually disabled client living in effective seclusion for at least five years. Chief Ombudsman Peter Boshier described this provision of care as “cruel and inhuman treatment… [which] could amount to a breach of the Optional Protocol to the Convention Against Torture”.
Any form of torture committed by the state should be of great concern us all, but the data highlight a particularly egregious and continuing trend among health services: an inability to treat Māori with the basic level of care afforded to non-Māori and required by international law.
Of people admitted to mental health units, Māori are two times more likely to be secluded than non-Māori, with Māori males aged 20–44 years having the highest seclusion rates of any group.
To put it bluntly, if you are Māori you are significantly more likely to be tortured by a government-funded public health service than if you weren’t Māori, or if you were in prison.
Fortunately, Māori aren’t well-known for letting a bad situation lie. Shocking outcomes such as these have fuelled generations of Māori to enter the Western-modelled public health system to push it towards culturally safe practices and compassion. Their efforts have regularly been met with debate and derision by non-Māori leaders, but their contribution and that of iwi-led healthcare providers continues to be pivotal to the success of public health campaigns and the vaccination push.
Taking our health into each others hands
Should Māori trust government agencies? Not without hesitation. Fortunately, Māori no longer need to trust only ‘Saint Ashley’ or his almost-exclusively-Pākehā, revolving-door leadership team in order to get trustworthy medical advice to be safe and healthy.
While ‘patient-centred care’ has become a buzzy phrase among global health leaders, iwi leaders have actually filled this role where DHBs have failed. Where leaders of the soon-to-be-axed DHBs have stood behind government ministers nodding their heads blindly, Māori have actually spoken directly to their communities in the words and vibe of their rohe.
Māori health researchers like Dr Rawiri Taonui, who helped create the wildly successful Te Whānau ā Apanui model, have come up with actual solutions to geographic challenges and distrust, such as vaccinating irrespective of age bands. This model reflects tikanga Māori healthcare at its best as it empowers whānau to come together for their collective health rather than rely on winning over each individual with communications designed from the perspective of self-interest.
The managing director of Te Kōhao Health, Tureiti Lady Moxon, leads 12 partner service providers throughout the Hauraki, Waikato, Maniapoto and Raukawa regions and has oversight of a medical centre and three satellite clinics in Hamilton and Raglan. Moxon recently told Stuff: “[We’re] trying to find new ways of doing things, with rangatahi using their platforms to reach others, incentives, and using mobile vaccinations.”
This is pivotal as it replaces a singular, very Pākehā narrative with something relevant to the people we are hoping to join us in the fight against Covid. While public health services in this country have a less-than-stellar history of treating and supporting Māori, services designed by and for Māori don’t share this troubled past and have shown the way to allay fears.
Health leaders like Lady Moxon and Dr Taonui have met people’s concerns with mana and reassurance about the kaupapa of the vaccine, rather than distributing blame or making offensive over-generalisations about the intelligence of scared people, scarred by a history of malpractice and marginalisation.
Haimona Gray (Ngāti Kahungunu ki Wairarapa) is a former Ministry of Health official and DHB spokesperson.
Image:
Shane Cotton, Coloured Dirt Dreaming from The Haymaker Series I-V (detail)
2012, Acrylic on linen.
Collections of Christchurch Art Gallery Te Puna o Waiwhetu and Dunedin Public Art Gallery (with funding from Dunedin Public Art Gallery Society)
Published with permission of Mr Cotton, supplied by Michael Lett gallery.
—
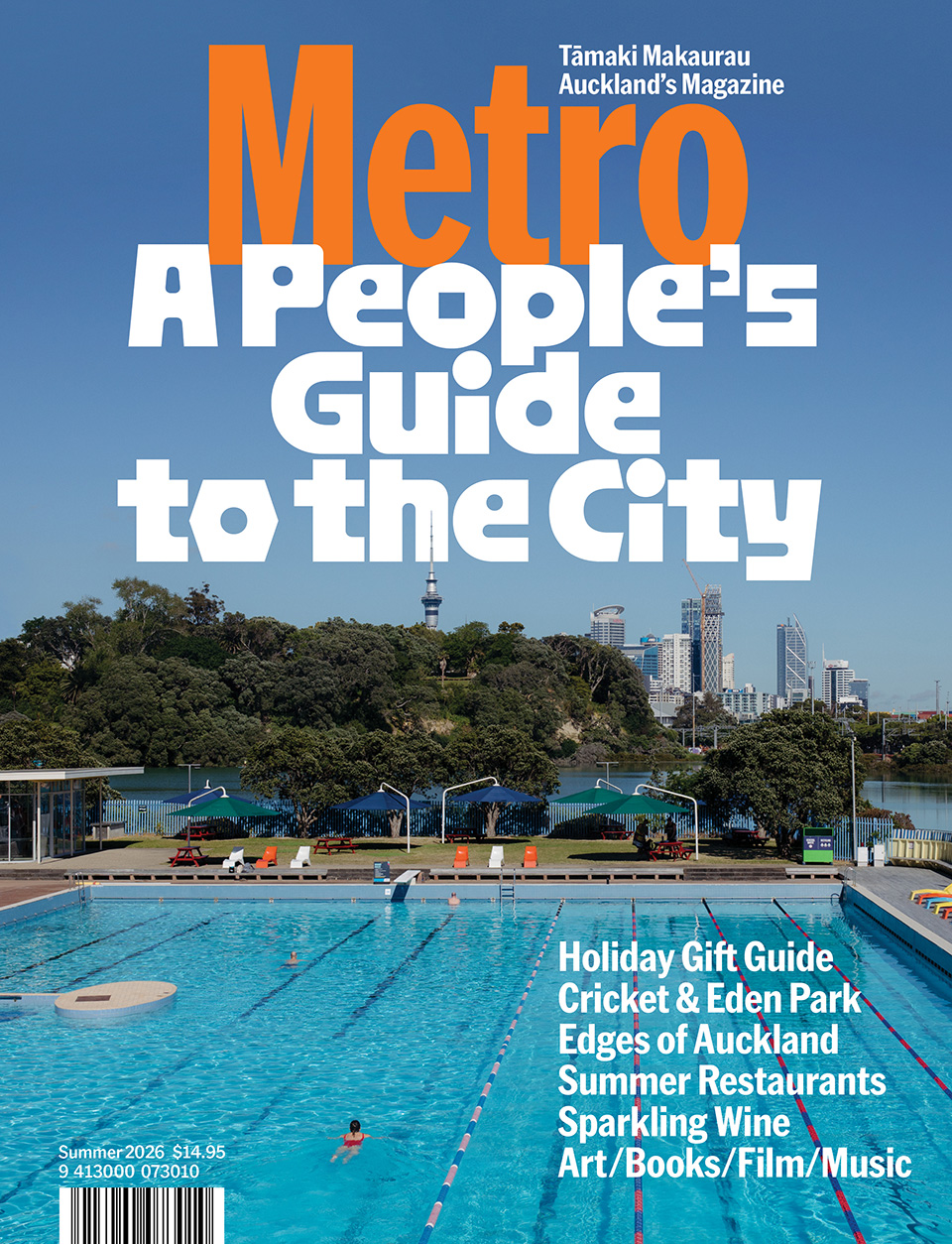
This story was published in Metro 433
Available here in print and pdf.